 A study just published (June 25, 2014) in the Journal of the American Medical Association,found that adding tomosynthesis (3-D imaging) to digital mammograms that analyzed the records of over 250 thousand women found a 10% reduction in the rate of “false positives” and recalls for repeat testing or biopsy and detected 41% more invasive cancers compared to digital mammogram alone.
A study just published (June 25, 2014) in the Journal of the American Medical Association,found that adding tomosynthesis (3-D imaging) to digital mammograms that analyzed the records of over 250 thousand women found a 10% reduction in the rate of “false positives” and recalls for repeat testing or biopsy and detected 41% more invasive cancers compared to digital mammogram alone.
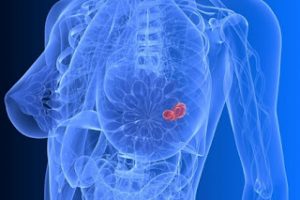
Finding invasive cancers earlier is an important step in treating breast cancers early. Enhanced detection of invasive cancers is especially important in young women and all women with dense breasts –that can hide behind dense tissue that is superimposed on it. While MRI of the breast and ultrasound can pick-up cancers not detected by routine mammography, they also lead to more “false positives” and are not optimal for screening.
Be sure to check as 3-D scans are not covered by all insurances and may be somewhat more expensive (usually less than $100.00). *false positive mammogram or scan result – radiology reading that notes an area or questions a “change” in an area of the breast that could be abnormal, but upon additional screening or biopsy is shown not to be cancer.
 Prostate cancer is a common and dreaded condition. The controversy over PSA testing, biopsy, and treatment continues to brew. Age, medical condition, and lifestyle are big factors in determining if, and how, prostate cancer is treated.
Prostate cancer is a common and dreaded condition. The controversy over PSA testing, biopsy, and treatment continues to brew. Age, medical condition, and lifestyle are big factors in determining if, and how, prostate cancer is treated. Last fall, a study published in the Journal of the American Medical Association (JAMA Int. Med. Aug. 5, 2013), showed a significant increase in the risk of developing breast cancer (perhaps double) when medications, known as calcium channel blockers (commonly used to treat high blood pressure), were taken over a long period of time. The increased risk appeared to be for two types of breast cancer – invasive lobular and invasive ductal cell types.
Last fall, a study published in the Journal of the American Medical Association (JAMA Int. Med. Aug. 5, 2013), showed a significant increase in the risk of developing breast cancer (perhaps double) when medications, known as calcium channel blockers (commonly used to treat high blood pressure), were taken over a long period of time. The increased risk appeared to be for two types of breast cancer – invasive lobular and invasive ductal cell types.